What is Trigeminal Neuralgia?
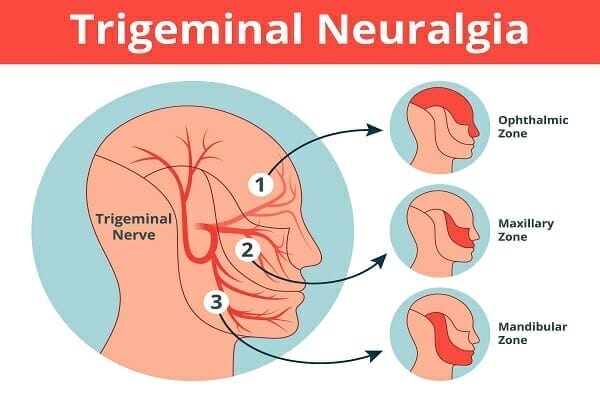
Trigeminal neuralgia (TN) occurs when the trigeminal nerve becomes irritated or compressed, often by a blood vessel pressing against the nerve at its base.
This causes abnormal signaling to the brain, resulting in severe facial pain. TN usually affects one side of the face and can involve areas such as the jaw, cheek, lips, or eyes.
Unlike ordinary facial pain, TN is episodic and can last from a few seconds to several minutes, sometimes recurring in clusters throughout the day.
Common Symptoms
The hallmark symptom of trigeminal neuralgia is sudden, severe facial pain, which may include:
- Sharp, stabbing, or electric-like sensations
- Pain triggered by light touch, chewing, talking, or even a breeze
- Episodes lasting seconds to minutes, sometimes recurring repeatedly
- Affects one side of the face, but in rare cases, both sides can be involved
Some individuals experience a “warning twinge” just before a full pain episode, helping identify potential triggers.
Pain Triggers
Trigeminal neuralgia is often triggered by everyday activities. Common triggers include:
- Chewing or biting
- Talking or smiling
- Brushing teeth or washing the face
- Exposure to wind or cold air
- Light touch or vibration on the face
Causes and Risk Factors
While the exact cause is sometimes unknown, TN is often linked to:
- Blood vessel compression on the trigeminal nerve
- Multiple sclerosis (can damage myelin around nerves)
- Facial trauma or surgery affecting nerve pathways
- Rarely, tumors pressing on the nerve
TN is more common in people over 50 and slightly more prevalent in women than men.
Diagnosis
Diagnosis is usually clinical, based on:
- Detailed patient history of pain episodes
- Neurological examination to rule out other conditions
- Imaging studies (MRI) to detect nerve compression or other structural issues
Proper diagnosis is essential, as facial pain can have many causes, including dental problems, migraines, or other neuropathic conditions.
Treatment Options
Treatment focuses on reducing pain episodes and improving quality of life. Options include:
1. Medications
- Anticonvulsants (e.g., carbamazepine) to reduce nerve firing
- Muscle relaxants or other neuropathic pain medications
2. Surgical Procedures
- Microvascular decompression to relieve nerve compression
- Gamma Knife radiosurgery (non-invasive)
- Rhizotomy procedures to selectively damage nerve fibers
3. Lifestyle and Supportive Measures
- Avoid known triggers when possible
- Gentle face care and oral hygiene to minimize accidental triggers
- Complementary therapies (physical therapy, relaxation techniques)
4. Neurorehabilitation
- Retrain nerve signaling pathways
- Reduce sensitivity to common triggers
- Improve facial motor control and coordination
- Enhance overall function and comfort during daily activities
This is exactly what we do at Cerebral Health, where every program is made to fit each person’s unique nervous system and needs.
Take control of your brain health today. At Cerebral Health, our personalized neurological care and proven strategies can help you manage symptoms, improve daily function, and support long-term wellness.
Schedule your complimentary consultation today and start your journey toward a stronger, clearer mind.

